Woody Allen once joked, “I’m not afraid of death. I just don’t want to be there when it happens.”
A world-wide survey by the Lien Foundation in Singapore recently reported the primary worry of the elderly is dying in pain. It listed England as the best place to die. Canada and the U.S. tied for ninth place.
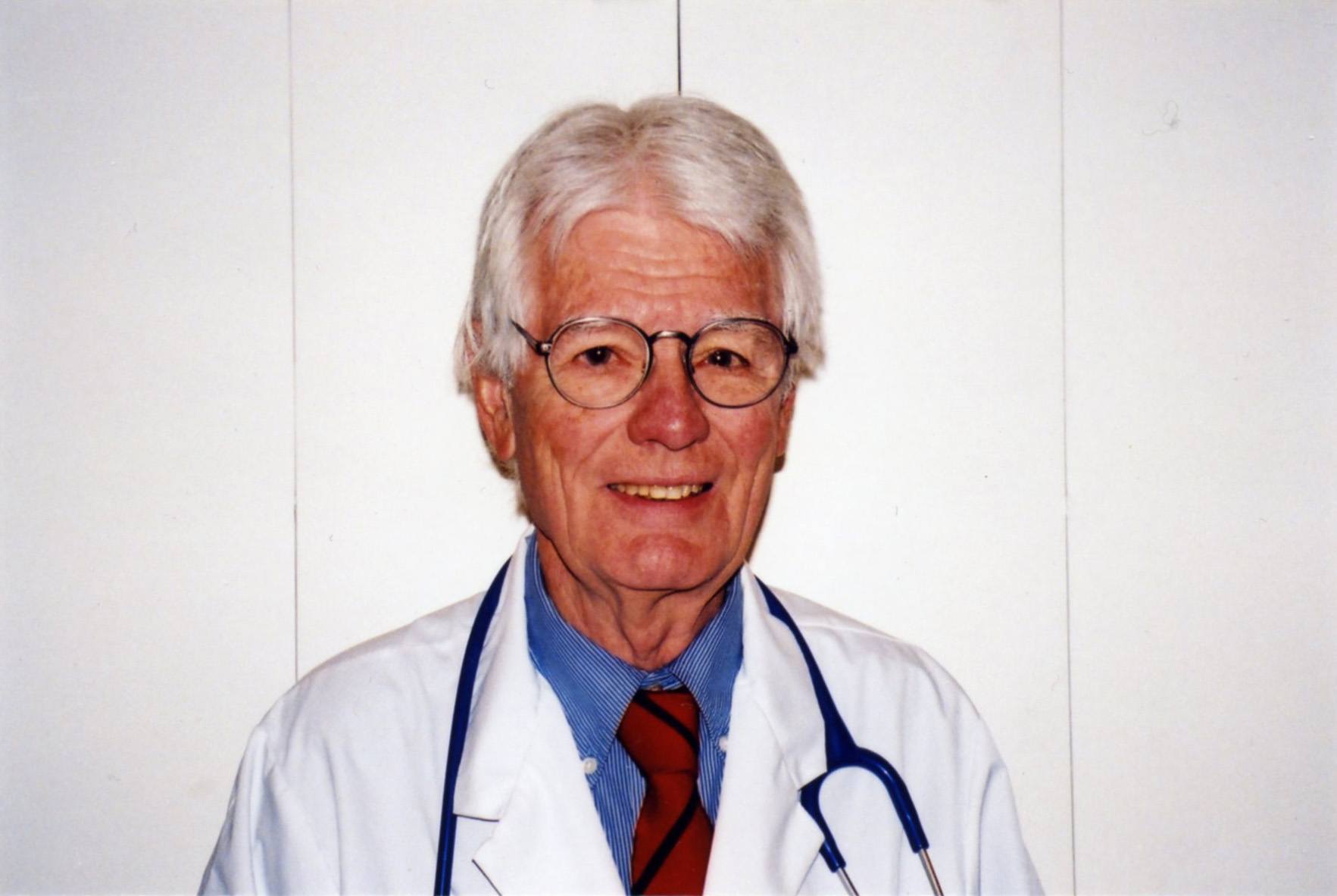
As a physician I’ve always known that pain is the overwhelming fear, particularly for cancer patients. I’ve also known that heroin has been available in Britain for 90 years to ease the final agony of death. This knowledge triggered a visit to England to witness its use and to question why it wasn’t used for this purpose in Canada. I didn’t realize my probe would engender so much controversy.
British pain specialists shot down the myths of heroin held by critics in North America. The most asinine is that terminal cancer patients become addicted to heroin. They don’t because it’s used for pain relief, not pleasure. But even if it did, who gives a tinker’s damn about addiction when patients have only days or hours to live?
Cancer specialists at Thomas’s Hospital in London told me some terminal patients were receiving 1,500 milligrams (mg) every four hours for pain, when five mg is the normal dose for post-operative cases. If patients experience a remission in their cancer they can be weaned off heroin in three weeks.
North Americans continue to claim that morphine is as good as heroin. But it’s a pharmacological fact that heroin is stronger, passes through the blood brain barrier faster and provides a sense of euphoria. I do not see anything wrong with giving dying patients a feeling of euphoria. Moreover, Scotland Yard told me that fears in Canada that hospital pharmacies might be broken into was nonsense, as it had not happened in Britain.
I reported these facts in my column and received thousands of letters of support. Then the unexpected happened. I was severely criticized by the Canadian Cancer Society, RCMP, The Pharmacy Association and some cancer specialists. I was uninformed, they insisted, and a headline-seeking journalist.
This began a five-year battle with critics during which time I formed the W. Gifford-Jones Foundation for Pain and received financial support from readers.
On Dec. 20, 1984, the government responded to public pressure and legalized heroin for terminal cancer patients.
But inane restrictions were imposed. Heroin had to be kept in guarded unknown locations in Canada and transferred to hospitals under police escort. Some hospitals required doctors to appear before a committee to present their case for heroin. These obstacles resulted in such small amounts of heroin being used by doctors that heroin is no longer imported into Canada.
My Foundation collected $500,000 which was donated to the University of Toronto Medical School to establish the W. Gifford-Jones Professorship in Pain Control and Palliative Care. This does an excellent job teaching the care of all terminal patients.
The Lien Foundation must be congratulated for creating a ‘Quality of Death Index.’
It considers the quality of death as important as the quality of life. But it should not depend on what country you live in or what part of that country, that determines how well you will be cared for in your final days.
It will take a mammoth effort for Canada and the U.S. to overtake England and other countries in this field. In Canada only 10 to 30% of those who need it receive end-of-life care.
Today we spend huge amounts of money on the battle with death that cannot be won. All too often I see terminal patients cruelly subjected to painful and useless diagnostic and so-called “therapeutic” procedures when what they need is pain-free hospice care.
Unfortunately Woody Allen cannot escape being there when death arrives. But there would be less fear for all of us if we knew that painkillers and palliative help would be available. Being number nine is not good enough for Canada or the U.S.
The long fight to legalize heroin is documented in my memoir You’re Going to Do What? See the web site www.docgiff.com For comments info@docgiff.com.