Twenty-two years ago Thursday – April 5, 1996 – then Vernon paramedic Don Devine and his partner got a call to go to a home on Mission Hill.
It had been a quiet, rainy morning, leading Devine to think the shift would be similar. All of that changed with one call, and changed Devine forever.
He and his partner were on-scene at the site of what turned out to be one of Canada’s worst mass killings, the slaying of members of the Gakhal family by Mark Chahal, who later killed himself in a Vernon motel.
Related: Gakhal/Saran anniversary reminds us of violence
“We got to the call and we were told that police didn’t know where the shooter was. That was my first indication guns were involved,” said Devine, who now lives in the North Shuswap, and reveals his story in a CBC TV documentary airing Sunday.
“There was a policeman inside, gun out, going from room to room. My partner immediately goes to a patient he has to work on. And I understood what was going on all of a sudden. A family was about to celebrate a wedding an estranged husband showed up with at least two firearms and murdered eight people; children, grandparents and everyone in between.”
Choking back tears, Devine had to continue on and assess what he and his partner were dealing with.
“I had to go and check whether this crumpled person on the floor was alive or dead. I had to go room to room. There were children…”
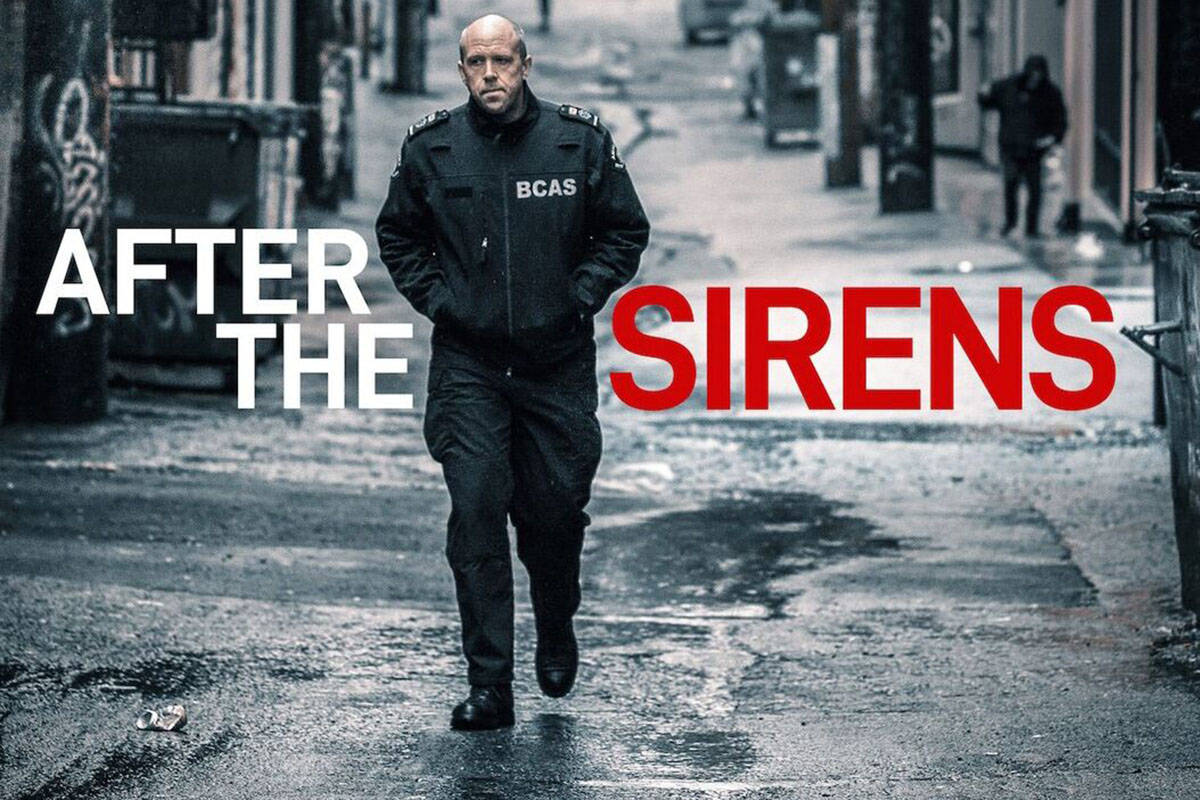
Devine and two other paramedics – one from Vancouver, the other from Ontario – are featured in a one-hour, riveting documentary called After The Sirens, produced and directed by Vancouver filmmaker Kevin Eastwood, which debuts Sunday at 9 p.m. on CBC.
Devine, Clive Derbyshire from Vancouver and Natalie Harris from Ontario talk about their dealings with Post Traumatic Stress Disorder (PTSD).
“All my energy drained out into the pavement,” Devine, a paramedic for 32 years, tells Eastwood of that Good Friday morning in 1996.
“I was confused, not understanding anymore. I remember saying very clearly to the supervisor, ‘call in a psychologist.’ There were six paramedics that were getting ready to go back for the second time to the scene in three different ambulances, already exposed to this.
“It took three hours for the clincial pyschologist to show up because he was busy. By then we were too sick. We didn’t want help, a lot of us. That very important first step didn’t happen. We call it the God Syndrome. You think you can save everybody. When you can’t, it’s hard.”
Derbyshire and Harris also share their experiences and dealings and sufferings with PTSD. Harris attempted suicide by swallowing pills, saved by a longtime friend. Derbyshire, who turned to methamphetamines to cope, contemplated taking his life as he walked over the Lions Gate Bridge.
Eastwood first met Derbyshire while filming an earlier documentary about Vancouver General Hospital’s emergency department.
“It was my first exposure to paramedics,” said Eastwood. I became aware that I was oblivious to the current situation and crisis with PTSD among paramedics. There was a general awareness about PTSD among first responders but the paramedics are really affected.
“Clive always seemed strong, impressive, powerful. I had no idea he was suffering from PTSD.”
According to the documentary, lots of people don’t know just how bad paramedics are suffering, and we learn that paramedics themselves either don’t say much or refuse to believe they’re suffering.
Eastwood introduces us in After The Sirens to Cheryl Drewitz-Chesney, author of PTSD Among Paramedics, and Vince Savoia, founder of TEMA, a PTSD support group named after a murder victim Savoia attended to as a former ambulance officer.
Drewitz-Chesney said in the general population across Canada, seven-to-10 per cent suffer PTSD. In paramedics, the number could be as high as one in four people, or 25 per cent, though the number could be higher as people may not be reporting.
Savoia says the national suicide average is 10 people per 100,000, yet the rate of suicide in the paramedic community is more than five times that average – 56 people per 100,000 (as of 2016).
Paramedics also have higher rates of PTSD than police officers and firefighters, even though they often go to the same calls. The author explains paramedics have longer and more intense exposure with patients.
Perhaps one of the most troubling aspects of the documentary is the revelation that even when paramedics do report PTSD, their claims are often not believed.
An Eastwood graphic shows there were 95 paramedic claims in B.C. in 2015. Only 13 were accepted.
“Something has to change there,” said Eastwood, who was told by another paramedic he should talk to Devine. He reached out to him and the pair met three times in 2017 to discuss Devine’s career for the film.
“He has seen more than his share of tragic scenes,” said Eastwood.
Today, Devine is a volunteer first responder auxiliary member, who still gets to go and help people, whose blood pressure and pulse rise each time he hears an ambulence siren. But he stays away from patient care.
And, as he admits on film, there are still triggers that he and other paramedics suffer from. In his case, mauve carpeting is an example that brings him back to that bloody Good Friday morning in Vernon.
“A lot of paramedics are sick because of it (PTSD),” said Devine. “They’ve taken their own lives. Their families are broken and gone. This is a society problem that is hugely expensive.”
@VernonNews
roger@vernonmorningstar.com
Like us on Facebook and follow us on Twitter.