Only two-thirds of eligible sexual assault survivors choose to undergo a “rape kit” and less than one-third subsequently hand over the forensic evidence to police, say researchers at an Ontario hospital with a dedicated emergency department program for victims.
“We see a significant volume of patients within our program and there’s great attrition in the rates of people who are going to pursue the whole justice side of things,” said Dr. Kari Sampsel, medical director of the Sexual Assault and Partner Abuse Care program at the Ottawa Hospital.
Across Canada, only 33 in every 1,000 cases of sexual assault are reported to the police; six lead to prosecution, of which three end in a conviction, says the study published online Tuesday in the Emergency Medicine Journal.
Hospital emergency rooms are often the first point of contact after a person experiences a sexual assault, say the researchers, who want to encourage ERs Canada-wide to step up efforts to help sexual assault survivors to secure justice in what is often a complex and stigmatizing legal system.
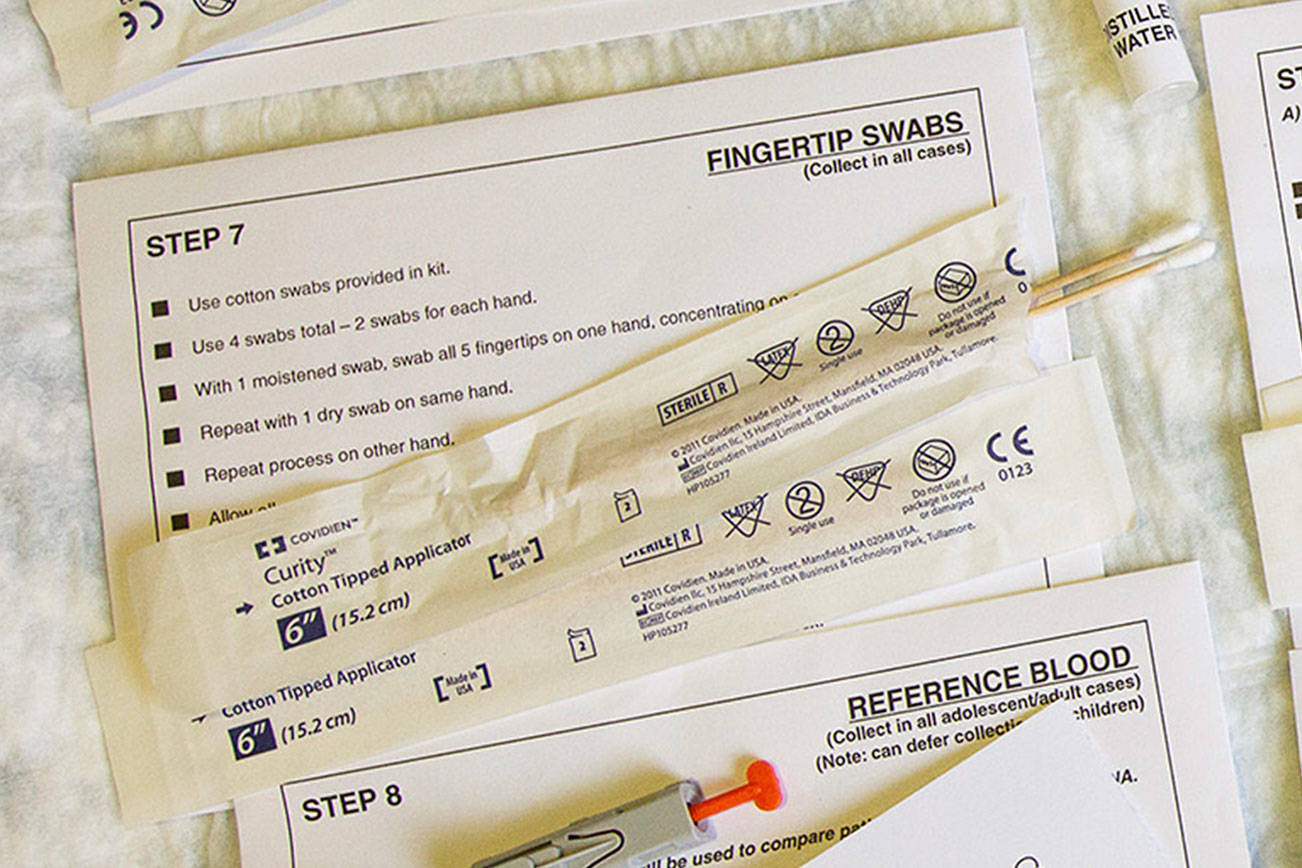
As part of the Ottawa Hospital program, sexual assault victims are offered the opportunity to undergo a rape kit — the collection of evidence that includes bodily fluids, fingernail scrapings and DNA samples, such as those left on clothing.
Me Too At Work: Sexual assault and harassment in the B.C. workplace
Yet many victims decline to go through the process, which can take eight to 10 hours and may feel like a second violation, Sampsel acknowledged.
“It can be very overwhelming for someone who’s been victimized,” she said, adding that there also can be fear about getting involved in the criminal justice system.
“People are afraid of what the process will be. They’ve seen this kind of case play out very publicly sometimes and they really don’t want to be part of something that’s going to potentially affect their life that much.”
The notion of bringing charges and going to court can be even more daunting when the assailant is an intimate partner, she said from Ottawa.
“So people may choose not to do that because that would completely blow apart their world … and they can’t afford to have their life disrupted in that way.”
The study, based on 2015 case registry data from the hospital’s program, showed 77 per cent of 262 patients who had been sexually assaulted were eligible for a rape kit, which must be done within 24 hours to 12 days after an incident, depending on the type of assault.
But only 129 of those who were eligible completed the process and just 60 subsequently handed over the forensic evidence to police, the study found.
More than 90 per cent of patients were female. Victims ranged from 16 to 80 years old, with an average age of 24.
Drugs or alcohol were involved in more than half of cases. This can affect recall of events, and is often used to undermine the survivor’s credibility in court, the researchers point out.
In almost 55 per cent of cases, the perpetrator was known to the victim or was an intimate partner. In 16 cases, several assailants were involved. Most assaults took place in the victim’s or assailant’s home, while one in 20 incidents occurred in student dorms.
Victims aged 16 to 24 were more than twice as likely to go through the rape kit process; those who didn’t know their assailant or were unsure of their identity were more than three times likely to release the rape kit evidence to the police, as were those who had been assaulted outdoors, researchers found.
Nicole Pietsch, co-ordinator of the Ontario Coalition of Rape Crisis Centres, said while forensic evidence is valuable in verifying that sexual contact occurred, it can’t prove it wasn’t consensual.
“Being able to prove that as a survivor, where the evidence is just based on your body or your narrative, is a really challenging thing to do, not because it didn’t happen necessarily but because there isn’t physical evidence in terms of consent,” said Pietsch, who was not involved in the research.
“The problems are not in the fact that they don’t wish to come forward. I would say the larger problem lies in the fact our criminal justice system doesn’t have the teeth often to be able to progress survivors’ stories in the way they can other crimes.”
Sheila Macdonald, director of the Ontario Network of Sexual Assault/Domestic Violence Treatment Centres, agreed that victims often feel the justice system isn’t going to serve their interests.
“They have their fears and self-blame … where somebody says ‘This happened because I was out drinking’ or ‘I shouldn’t have invited him home,’” she said. “So those myths are already out there and they’re internalized in people, so there’s a huge reluctance to come forward and report.”
Macdonald, who works out of Women’s College Hospital in Toronto, said the barriers that make victims reluctant to come forward need to be addressed, including those posed by the criminal justice system.
“What is it in the structure and the system that’s creating these barriers that somebody who can be so violated can say ‘I can’t come forward?’
“That’s where our focus needs to be.”
Sheryl Ubelacker, The Canadian Press